Roads to a Medical Neighborhood
The Center for Rural Health and Social Service Development Brings New Vitality to the Region
Aspects Volume 38 No. 4
Written by Karen Carlson • Photography by Jason Johnson
 In 2009, Dean Dorsey added "service to the community" to the mission statement. Those four words weren't just an afterthought: Years of planning have lead to a thriving Office of Community Health and Service, led by Associate Dean David Steward, MD, MPH, former chair of Internal Medicine. "This office has helped solidify SIU as a leader in the community," Dr. Steward says.
In 2009, Dean Dorsey added "service to the community" to the mission statement. Those four words weren't just an afterthought: Years of planning have lead to a thriving Office of Community Health and Service, led by Associate Dean David Steward, MD, MPH, former chair of Internal Medicine. "This office has helped solidify SIU as a leader in the community," Dr. Steward says.
The Office of Community Health and Service, or OCHAS, has worked within the School of Medicine and externally in communities throughout downstate Illinois to achieve successes on all levels of community health within the 66 Illinois counties the office reaches.
Using SIU School of Medicine's existing outreach programs and adding new ones, the OCHAS team is building a "medical neighborhood," a term coined by primary care medicine to reflect attributes of a patient-centered medical home. The OCHAS staff is taking this concept into the towns of central and southern Illinois with the strategic placement of regional offices in southeast central Illinois, western Illinois and southern Illinois. "These offices reflect SIU's robust commitment to working with these communities," Dr. Steward says. Single-staffer sites in Mattoon and Havana are initiating work that may mirror a long-standing and highly successful outreach office in Carbondale: the Center for Rural Health and Social Service Development.
Right Image Caption: Jeff Franklin, Ruth Heitkamp, Tom Bik, Dennis Presley, Jennifer Cutrell, Kath Doan and Kim Sanders.
Center for Rural Health
The Center for Rural Health and Social Service Development (CRHSSD) has a big name, a big job and provides big rewards. Formerly under SIUC's Office of Regional and Economic Development, the center moved under the stewardship of the School of Medicine in 2012. It recently moved its office to Wheeler Hall on the SIUC campus. The Center, approved by the Illinois Board of Higher Education, represents the southern most 22 Illinois counties.
What began as a small resource center in 1989 has evolved into a robust system office of a dozen people, including four graduate assistants.
Executive Director Kim Sanders says that southern Illinois, which includes 16 counties in the Illinois Delta Region, is comparable to the Delta regions of Mississippi and Alabama with similar poor health outcomes. The 2015 County Health Rankings and Roadmap Report ranks 20 of the 22 southernmost counties in the lower 50th percentile of Illinois counties for health outcomes when looking at morbidity and mortality measures; 16 of those counties are in the lower 75th percentile. (countyhealthrankings.org).
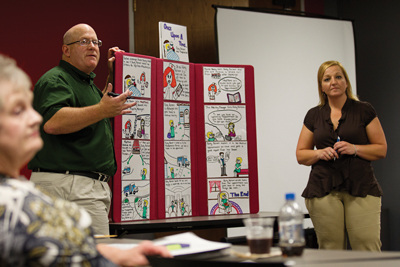 Left Image Caption: At a recent meeting, Dennis Presley and Tracey Johnson of MedTrans draw storyboards to help hospital administrators visualize the idea process.
Left Image Caption: At a recent meeting, Dennis Presley and Tracey Johnson of MedTrans draw storyboards to help hospital administrators visualize the idea process.
The Center's mission is to strengthen the infrastructure and collaborations in the region to enhance its residents' health. It does everything from helping clients understand the electronic health record, implementing the patient-centered medical home and writing grants. "Many people don't know how to approach experts in areas like geriatrics, transportation or child health," Sanders says. "We can put together some cool projects that benefit the entire region across many disciplines." She notes that many places don't have the administrative support to pursue grant funding. "We can pull people together and clear the red tape to let people do what they're good at. It's not just university collaboration, but also community collaboration. We can bridge the cultural gap. We work here and grew up here."
They are also health care advocates. They've recommended policy alternatives that have led to changes in rural medical transportation and assisted in policy-related symposiums for child welfare and veterans' benefits. They've published and presented research on topics such as telepsychiatry, patient navigator programs, the Patient-Centered Medical Home and coordinated school health implementation.
Collaborators agree. "The Center for Rural Health and Social Service Development has been a key feature in the health landscape of southern Illinois for many years," says Miriam Link-Mullison, administrator for the Jackson County Health Department.
"We have a common philosophy of leveraging increased community engagement and facilitating problem solving in the regions mutually served by Southern Illinois Healthcare (SIH) and SIU," says Woody Thorne, Vice President of Community Affairs at SIH. "The Center has been a catalyst for the SIU School of Medicine and the broader SIUC campus to be engaged with SIH and many community partners in bringing about new and innovative solutions to the challenges facing the rural Illinois Delta region."
Focusing upstream over the past 20 years, the Center has made an impact. According to Sanders, in FY '15, the internal rate of return on the investment (ROI) is 270 percent. The regional ROI is 464 percent. "For a small amount of money the university invests, the ROI is big." FY '15 grant submissions total $1.5 million. Much of that funding is pushed back into the community through grants to agencies to fund projects ranging from enhanced EMS training to workplace health program development. Among the numerous projects are two flagship projects ñ the longest running and most successful: the Rural Medical Transportation Network and the Coordinated Approach to Child Health (CATCH) program.
Rural Medical Transportation Network
Access to care is an ongoing issue in southern Illinois. At least 10 percent of residents say they miss medical appointments, according to Rural Medical Transportation Network Project Coordinator Dennis Presley. He once got a call from an elderly woman who lived just outside St. Louis. "She couldn't get to her neurology appointment. Even though she lived in an urban setting and was just a few miles away, she couldn't get there."
Other people, he says, would schedule more appointments if they had reliable transportation, and health care providers are frustrated. "They are emotionally attached to their patients, and it costs more money to treat them when they are sicker." A 2013 survey by the project found that people still have reservations about using public transportation and many don't understand how to use transportation. "So they sit at home and get sicker," Presley says.
"Our goal is to identify patients who need help with medical transportation and prevent re-hospitalizations," Presley explains. It seems like a simple enough task, but as Presley describes, extensive research has uncovered a tough, multi-layered and complex issue. It's unusual, Presley says, for hospital, EMS and transit to talk to each other. "When they are prompted to do so, they understand they can do things to help each other."
Planning between the Rural Medical Transportation Network and several transit districts in the region initiated MEDTRANS, a unique project in Illinois. MEDTRANS is a free service in which staff of a collaborative project work with hospitals and health centers to identify patients in need and coordinate access to medical appointments after hospital discharge. This could mean simply rescheduling appointments to align with the bus schedules.
Another innovative project is Mobile Integrated Health Care, which is designed to help high-risk patients achieve a good quality of life and save money. In this promising model, EMS providers visit patients' homes to do wellness checks. "Some patients call EMS even though it is not an emergency. This model gives them care without the high-priced hospital or ER visit," Presley says. The cost, about $75 a call, could prevent hospital readmissions, keep patients at home and healthier and generate more revenue for EMS providers. A key feature of the patient/provider relationship - trust - is already established, Presley says. "Most patients in these small towns know their EMS providers; they've called the ambulance before. They don't mind them coming into the house."
The Center's Rural Medical Transportation Network is on the leading edge of this model nationwide. Presley, who works part time as a police officer, enjoys the innovation. "Nobody else is doing things like this. It's replicable and has a good chance of changing our system of health care as a whole.
Through the Rural Medical Transportation Project, Presley was able to make arrangements to get the East St. Louis woman get to her neurology appointment. "She was at the end of the rope, and our program helped her overcome barriers. That makes us feel pretty awesome."
CATCH
Illinois is one of only a handful of states that still requires daily PE for all K-12 students. "But schools have many ways that they can opt out of it," says Jeff Franklin, project coordinator for the CATCH program. Time and testing requirements prevent schools from implementing health programs, he says. "If we would take the time to create healthier school environments and improve the health of our children, we would see students that move more, score better, test better and behave better." CATCH implements four core components in the school environment: nutrition program, physical education program, curricula and family education.
Franklin has spent his career building partnerships with schools, health care centers and public health departments to create a generation of children to whom health issues such as obesity, cardiovascular disease and bullying are things of the past. Funded by a grant from U.S. Health Resources and Services Administration (HRSA), the CATCH project covers 16 counties in Illinois, part of the 252-county Delta Region.
Franklin and his team have expanded the school health initiative to incorporate all eight components of the CDC's coordinated school health model, as well as including social and emotional aspects of health. As a result, more than 80 percent of grade schools in the Delta region - about 20,000 kids - have benefited from an evidence-based, coordinated school health program. "Our goal is to get 100 percent," Franklin says.
The HRSA funding allows the CATCH program to purchase the curriculum and equipment for the schools. The CATCH team, in order to effect a Policy, Systems and Environmental change, serve on school wellness committees, create implementation action plans, help with district- wide wellness policies and include staff health in order to work successfully in partnership with school boards. The grant supports a network of team members from health departments and Southern Illinois Healthcare. Departments at SIUC and the School of Medicine are collaborators as well.
 464% - The Return On the Investment for the Southern Illinois region from the Center
464% - The Return On the Investment for the Southern Illinois region from the Center
"The U.S. Health Resources and Services Administration wanted us to show that we were improving physical activity levels: 50 percent of our children in CATCH schools have improved their physical activity levels." Franklin says. Schools say their culture has changed to an environment focused on the health and wellness of the students. "Now there's a focus on ëwhole child, whole community' approach," Franklin says.
For Woody Thorne of SIH, the CATCH program is the most successful collaboration. "SIH, health department staff and the CATCH consortium have all worked hard to make CATCH a success. "It has become an effective tool to integrate public health principles, particularly related to physical activity and nutrition, into the entire population."
Like the Rural Medical Transportation Network, the CATCH program is a model for the state and the nation. Franklin credits the strong team partners who provide the structure that doesn't exist in other coalitions. "We realized we can't do it without each other. We have to pool our time and talents and resources and move forward."
For Franklin, a former University of Illinois Extension youth development educator and health educator, the impact on the kids is the greatest reward. He recalls a young boy who cried when winning a bicycle at a CATCH-funded health and wellness family event. "His parents didn't have the resources to purchase a bike. So this was an exciting opportunity for him to increase his physical activity. He rode that bike everywhere."
Geriatric Program
The Center is very excited about its latest endeavor: A collaboration with HRSA and Rush University to establish a geriatric workforce enhancement program. The goal is to educate providers on the need for enhanced services for the elderly population. "We have a higher rate of geriatric patients in southern Illinois and a shortage of primary care providers, including social workers, physician assistants and nurses," Sanders says. "Providers in training need education about how to manage the chronic conditions of seniors."
This grant, awarded in July 2015, will be integrated in Family and Community Medicine residency in Carbondale. The residency program will work to make their clinic more geriatric-friendly. A geriatric fellowship is on the wish list.
The ideas are just starting to bubble to the surface: What if every first exam room was designated the geriatric room? What if we had exam tables lowered so patients could easily sit on them? What if employers had health programs so employees retired healthier?
Project Coordinator Ruth Heitkamp is beginning to organize a steering committee to discuss more ideas for palliative care, hospice and home health. "We need to see where the gaps are, get big employers to buy in to the concept and create a regional plan to address geriatric care."
Heitkamp says it's building on the notion of a medical neighborhood. "You have to look at all the players in your region, from hospitals and clinics to law enforcement, emergency responders and medical personnel, all these people have to work together corroboratively to get change." Southern Illinois has been working on this concept since the Center started.
As many suburbanites will tell you, successful neighborhoods begin with neighbors who know and support each other. CRHSSD staff are the neighborhood leaders, bringing people and partners together to start conversations and build relationships to strengthen the growing medical neighborhood of southern Illinois. "We are here to serve our community. We want to help our partners make southern Illinois an even better place to live," Sanders says. "After all, we live here, too."
Stronger Neighborhoods
To help strengthen the medical neighborhoods of central Illinois, the Office of Community Health and Service in Springfield has opened three new outreach offices in Havana, Mattoon and Springfield.
The goals of the offices are much like the Center for Rural Health in Carbondale: to link together the resources available within the region. This includes the health-care system, economic efforts, social services, populations and sub-populations, local governments, public health jurisdictions, public school systems and other components in the context of regional health. Projects may include everything from helping agencies find food resources to assisting hospitals with the required Community Health Needs Assessment. The office hopes to develop regional councils to plan, develop and implement programs to address barriers to local and regional health care.
Brent Todd, a resident of Charleston who grew up in Ridge Farm, is the assistant director for Regional Medical Programs and Rural Health in Mattoon. Laura Hepp Kessel, a resident of Canton, originally from Perry County in southern Illinois, is the assistant director for Regional Medical Programs and Rural Health in Havana.
"SIU School of Medicine has so many resources available to assist in improving the health of the region. These offices will build relationships that link SIU services to the people who need them," Dr. Steward said. "We want to grow a professional network of providers to improve health in all aspects of life."